Until now, ground ambulance and medical flight paramedics alike did not have a specific guideline to follow when treating patients with syncope. Syncope, otherwise known as fainting, happens when there’s a lack of blood supply and the blood pressure drops to deprive the brain of oxygen. And now the American College of Cardiology has released a guideline to help you understand the best course of action to take when encountering such patients.
What to do When You Encounter a Medical Flight Patient with Syncope
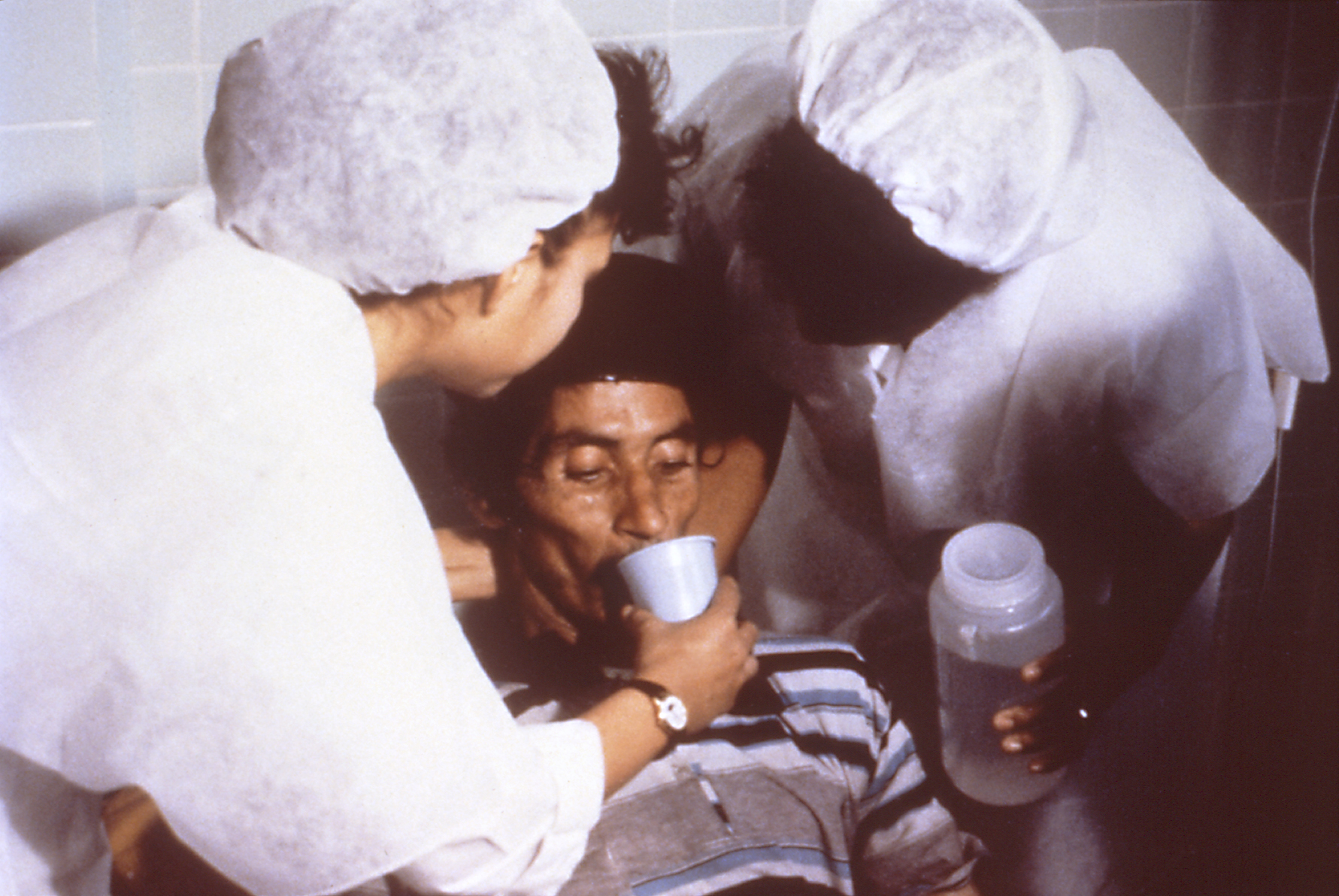
When you respond to a situation in which a patient has fainted, here’s what you need to do:
- It’s crucial that your initial evaluation includes a detailed physical examination and medical history. This will help you identify whether there are any possible underlying conditions that could result in the fainting.
- Fainting usually occurs while standing when there’s a drop in blood pressure, as this reduces oxygen supply to the brain. In most cases, the condition may not be life-threatening. So you should do your best to try and ease the worries of your patients.
- If your medical flight carries a portable ECG, it’s best that you use it during your evaluation. This will help you determine if there’s any abnormality that requires treatment.
- During your evaluation, if you find out that the patient has a serious medical condition that possibly caused the fainting, it’s crucial that they are transported to a hospital immediately. This holds true even if the patient seems to be recovering fine from the fainting.
- You can rule out the need for unnecessary evaluations such as routine lab testing and routine cardiac imaging such as CT scan or MRI unless you suspect the patient has a cardiac issue. There’s also no need for carotid artery or head imaging unless you need to perform a further evaluation.
These are some of the important guidelines to follow when encountering patients with syncope. Watch out for the next post to find out more.